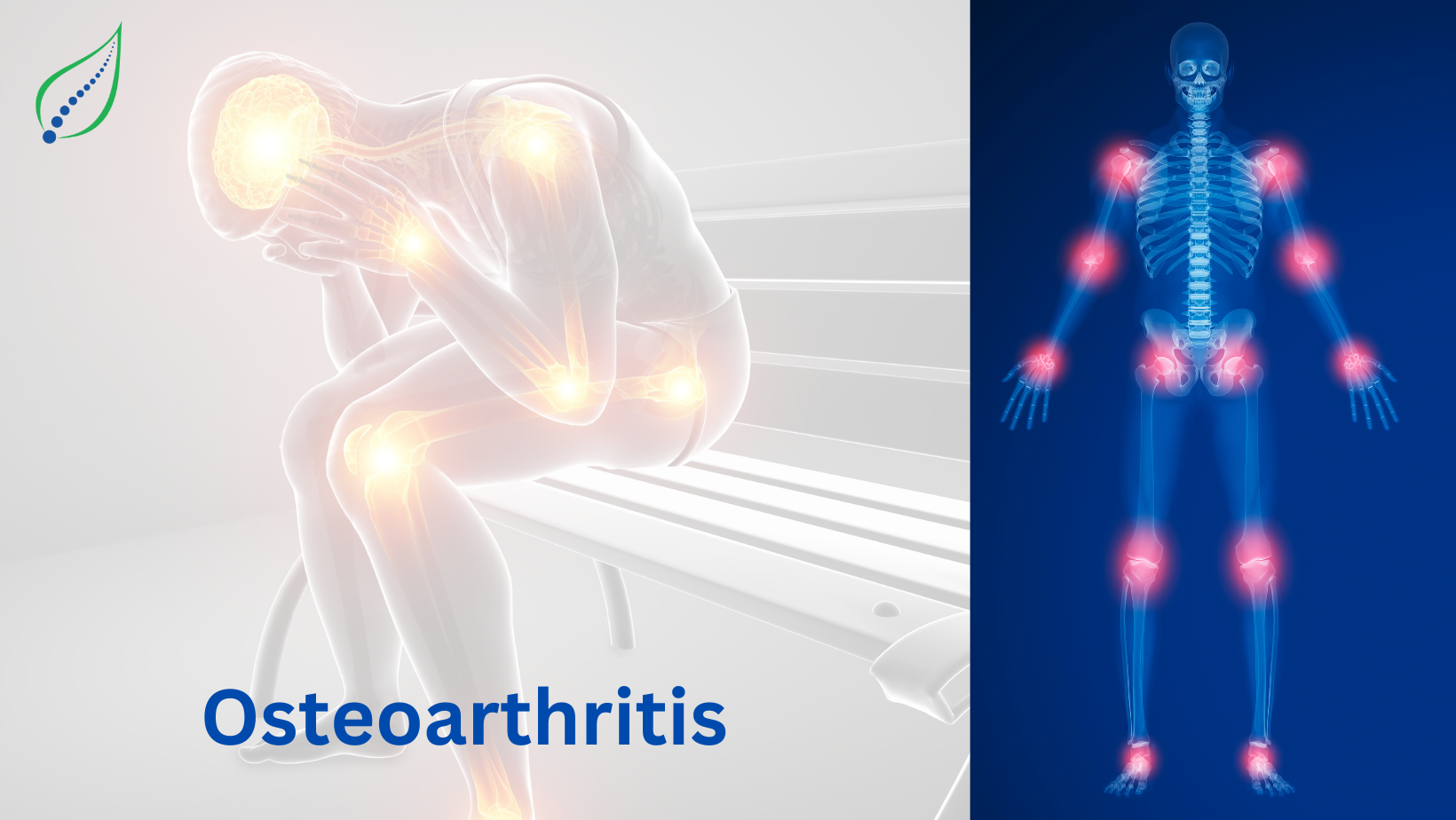
Osteoarthritis
Age related degenerative wear & tear of the joint cartilage results in osteoarthritis(OA). OA presents with joint pain, stiffness & loss of joint function. Degradation can be seen with cartilage, changes in shape of the bone and synovial inflammation.OA can be monoarticular or polyarticular in presentation with the affected joints in different stages of disease progression.
It typically affects the proximal and distal interphalangeal joints, first carpometacarpal (CMC) joints, hips, knees, first metatarsophalangeal joints, and joints of the lower cervical and lumbar spine. Risk factors for developing OA include- Age, Female gender, Obesity, Anatomical factors, Muscle weakness, Joint injury (occupation/sports activities).
Types Of Osteoarthritis:
- Primary OA - No pre-existing disorder but is associated with risk factors
- Secondary OA - Includes risk factors along with other predisposing factors
Pathophysiology:
Changes are seen in-
- Earliest changes occur at the level of the articular cartilage- surface fibrillation, irregularity, and focal erosions.
- After cartilage injury, collagen matrix is damaged, causing chondrocytes to proliferate & ossify resulting in formation of osteophytes.
- Improperly mineralized collagen in advanced stages causes subchondral bone thickening & bone cysts occur. In rarer cases, bony erosions can also be seen.
- In end-stage OA, synovial inflammation & hypertrophy occurs due to deposition of calcium phosphate and calcium pyrophosphate dihydrate crystals within the joint.
Symptoms -
- Joint pain on movement
- Joint stiffness in the morning or after rest
- Reduced ROM
- Muscle weakness
- Swelling
- Crepitus during movement
- Patients with chronic pain present with continuous pain, deformity, instability
Clinical Findings:
- Bony enlargement
- Crepitus
- Effusions (non-inflammatory)
- Limited range of motion
- Tenderness at joint lines
- Pain upon passive motion
- Heberden’s nodes (posterolateral swellings of DIP joints); Bouchard’s nodes (posterolateral swellings of PIP joints), and squaring at the base of the thumb (first CMC joints) in OA Hand.
Investigations:
XRAY- Narrowing of joint space, osteophytes, and sometimes changes in the subchondral bone can be seen
MRI- To rule out other causes of joint pain
Since OA is non- inflammatory, lab findings appear to be normal.
Joint effusion aspiration rules out septic arthritis, gouty arthritis, etc.
Treatment -
- Medications- NSAID's, COX2 inhibitors to reduce the pain.
- Joint aspiration in case of joint effusion
- Intra-articular injections- Intra articular therapeutic steroid or hyaluronic acid injections can be given which provide symptom relief.
- Physical Therapy- Exercises to improve joint range of motion, muscle strengthening & stretching, joint & soft tissue mobilization
- Braces- For those with joint instability & varus or valgus misalignment, brace support should be considered. Heel wedges can also reduce medial compartment load.
- Weight loss- Patients with OA knee & OA hip should participate in weight loss programme through diet & exercise.