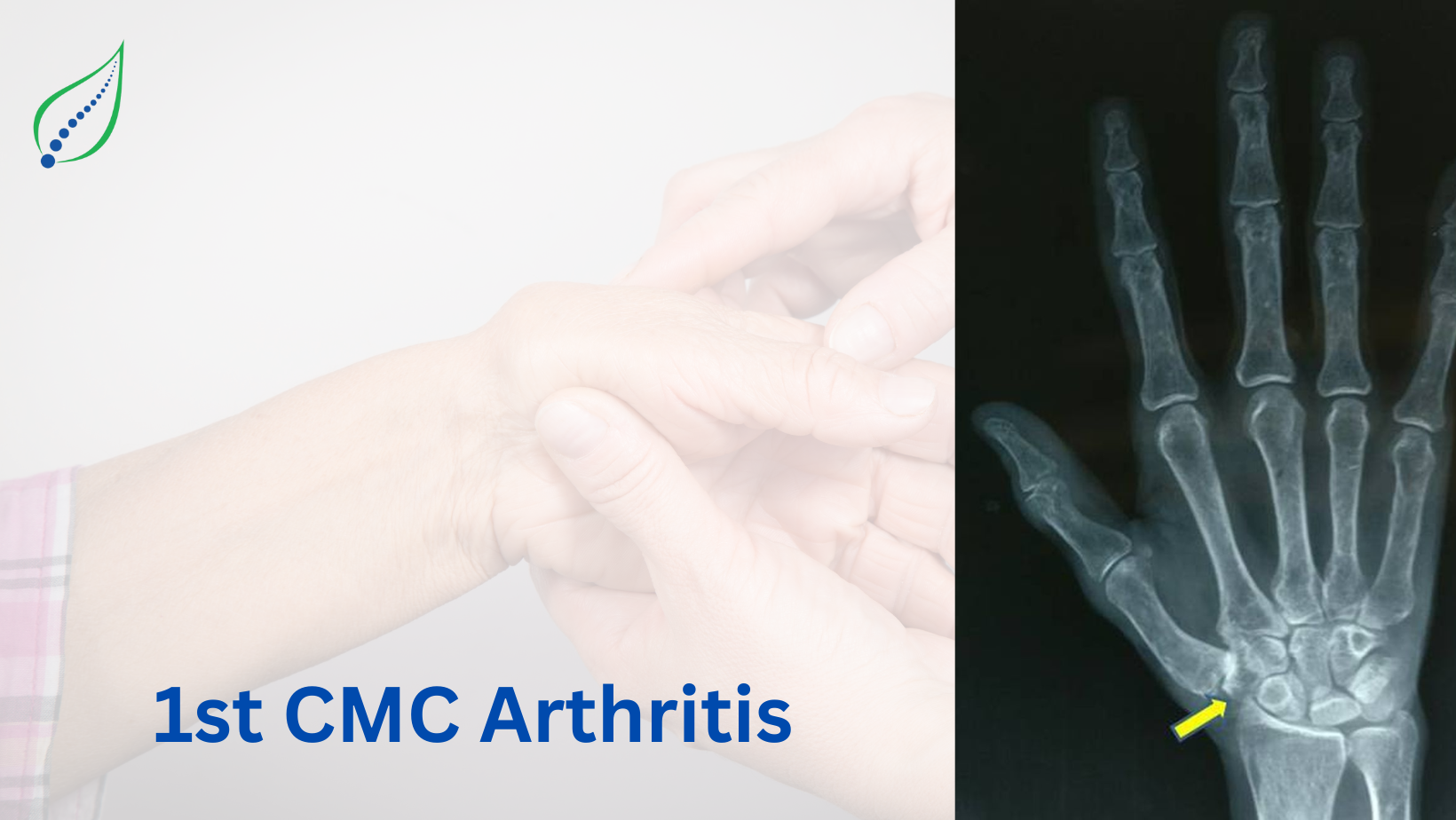
1st CMC Arthritis
The first CMC or thumb metacarpal is a saddle joint with biconcave - convex joint surface. The biconcave surface is formed by trapezium carpal bone and convex surface is formed by first metacarpal of thumb. The trapezium carpal bone shares it concave surface with trapezoid, scaphoid and second metacarpal bone. There are 4 ligaments that provide major stability to joint are Anterior oblique ligament, dorsal radial ligament, posterior oblique ligament and inter carpal ligament. The most important stabilizer against valgus stress is the anterior oblique ligament, due to this biconcave articulation the first CMC joint lacks bony confinement and to stabilize the joint anterior oblique ligament also known as BEAK ligament plays a key role. The laxity of the beak ligament leads to increased stress load on the CMC joint leading to cartilage loss, bony impingement and pain. The cartilage loss is mainly due to lose of glycosaminoglycan from extra cellular matrix which aggravates the arthritis condition. The CMC joint allows ROM in three different planes – 40 0 to 70 0 thumb adduction-abduction perpendicular to the plane of the palm, 40 0 to 50 0 thumb flexion-extension parallel to the plane of the palm, axial rotation. Based on the factors like structure, laxity first CMC joint is prone for degeneration and contributes second most degenerative joint disease of the hand. There is a study which says that First CMC OA affects post-menopausal women in their 5th to 6th decade of life due to hormonal predisposition.
Eaton classified first CMC OA into 4 stages: These stages are classified by using radiographs and Arthroscopy
- Stage I- Normal articular cartilage with possible joint widening due to effusion and laxity of beak ligament
- Stage II – Narrowing of joint space, debris and osteophytes smaller than 2mm in size with more than 1/3 subluxation of metacarpal
- Stage III - Shows more severe joint narrowing with osteophytes and debris >2mm in size
- Stage IV – Begins when there is involvement of the scaphotrapezial joint
SYMPTOMS
- Pain in the thumb joint during activities of daily living
- Difficulty in pinching and gripping
- Weakened pinch strength
- Stiff thumb
- Axial compression of the metacarpal upon carpal bone produces a griding sensation
- Arthritic Thumb shows Knobby Deformity
CAUSES
Primary factors
- Chronic, high compressive loads
- Unstable joint or ligament laxity
- Complex ROM
Secondary factors
- Gout
- RA
- Infection
- Trauma
DIAGNOSIS
- Radiographs are primary assessment tool to see the degeneration of the articular surfaces of the 1st metacarpal and trapezium which appears as joint space narrowing, bony spurs and subluxation of the first metacarpal off the trapezium with adduction stance.
- Physical Measurements - First CMC joint ROM, Grip and pinch (tripod & key), Strength and Dexterity, these are done by using NK hand assessment system, dynamometer and pinch gauges.
TREATMENT
- Conservative treatments are started in Eaton stage I disease with activity modification, advising splints, slings, non-steroidal anti-inflammatory drugs, cortisol injection;
- In some studies, it is proven that intra-articular steroid injection of first CMC 80% effective with pain relief; 25% effective in stage IV; But sometimes dependent on injections leads weakening of joint.
- ROM and strengthening exercise for thumb.
- Strengthening exercise for intrinsic and extrinsic muscles of thumb and fingers
- Application of therapeutic ultrasound, TENS -these modalities has healing property to heal articular cartilage, Phonophoresis helps in production of hyaluronan.
- Dry-needling helps in reducing pain.
- Some studies proven that combination of joint mobilization, neural mobilization and CMC joint exercises effectively relieves pain.